
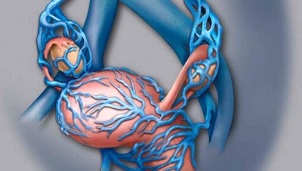
Both men and women are prone to varicose veins, but the weaker ones often do not suffer from the consequences of the disease. The most common mention of varicose veins is associated with swelling of the veins in the legs below the knee, but there is a case of varicose veins in women. It is a fairly common disease that is endangered by all women during childbearing.
Most pelvic varicose veins occur in women who do heavy physical work or during pregnancy. This is due to the increased stress in the woman’s body, which causes increased venous pressure, which provokes varicose veins in the hips.
Sudden abdominal pain is the first symptom of pelvic varicose veins.
Visceral varicose veins are especially dangerous for pregnant women and this is one of the main reasons for prescribing a cesarean section. Doctors explain this by saying that natural childbirth can cause bleeding and endanger the lives of both mother and child. The occurrence of this disease during pregnancy is due to the fact that the enlarged uterus is compressed and interferes with normal blood circulation. Increased hormone levels also contribute to the formation of varicose veins in the small pelvis.
Due to changes in hormonal levels in mature women, the disease can begin to develop during puberty. Complicating the situation is that it is quite difficult to detect varicose veins in the pelvis because the disease that develops at this stage of life is rarely accompanied by obvious symptoms. An indirect reason for the specialist's visit may be the increased release of the female reproductive system.
In women, pelvic varicose veins often occur during sitting in the office. This is due to the loss of plasticity of the venous walls due to the low mobility of the person. Men are also susceptible to this disease, but much less frequently than women.
The most obvious symptom of pelvic varicose veins may be lower abdominal pain, especially when standing when the body is straight. It can often cause pain through intercourse or other intense stress on the body. In addition, varicose veins can spread from the pelvis to the perineum and gluteal region.
Experts call the pelvic internal varicose veins a complex disease. This is due to the difficulty of diagnosis, as the onset of the disease does not have as many symptoms and is not clearly manifested. The timeliness of detecting varicose veins gives hope for complete recovery. There is also a high chance of making a misdiagnosis in the early stages of the disease.
Main causes of the disease

Poor heritability can be a problem.
Connective tissue dysplasia is considered a sign of their pathology, which causes varicose veins in the pelvis. These problems are often caused by poor inheritance, but people whose lives are combined with the following factors can also suffer from varicose veins:
- Office work or other sedentary occupation;
- Heavy physical activity when the body is not pre-prepared for them;
- Irregular sexual activity;
- High estrogen hormone;
- Gynecological diseases of women, common inflammation;
- Tumors near the internal organs.
Studies have shown a link between the use of contraceptives and other hormonal medications and the occurrence of varicose veins in the small pelvis.
The coverage of this disease in pregnant women requires special attention. Unfortunately, in up to 30% of cases during this period, diseases are observed in women. Doctors tend to believe that pregnancy can give a boost to the development of connective tissue dysplasia in the female body, leading to varicose veins.
In women, varicose veins occur due to an increase in the number of female hormones, which have a similar effect on the body when using contraceptives. This is exacerbated by the pressure on the internal veins of the pelvis during fetal development, which causes increased compression. Additional pathways of blood outflow develop that are no longer required after delivery and require a recovery procedure to eliminate them.
A prenatal clinic that is about to register has a risk group that includes women who are prone to inflammation of the reproductive organs. Pregnant women with high estrogen levels also require special attention.
Symptoms of the disease

The main symptoms of pelvic varicose veins include more frequent pain in the lower abdomen and abundant secretions from the genitals. But there may be other reasons for these signs, which is why it is so difficult to diagnose such pelvic varicose veins at an early stage.
Indirect signs include the detection of swollen veins in the buttocks and perineum. In some patients, abdominal pain increases in the first days of the menstrual cycle.
The main symptoms of pelvic varicose veins in women are:
- Pain before worse than usual menstruation;
- Menstrual disorders;
- Enhancement of sensitive sensations in the perineal region;
- Pain radiating from the lower abdomen to the lower waist;
- Increased vaginal sensitivity;
- Frequent urination;
- Severity in the lumbar spine in a prolonged standing or sitting position.
Depending on the stage of development of the pelvic varicose veins and the individual characteristics of each woman, several symptoms can be observed at the same time, or each separately. In any case, if you notice any of the signs listed, visit your gynecologist’s office.
Diagnostic Methods
There are several methods for detecting and diagnosing varicose veins in the pelvic organs, but Doppler ultrasound is considered predominant. Using this procedure, it is possible to identify the outlines of the veins with ultrasound waves and project them onto the screen of the device or take a photograph. The image allows you to detect all the deformation sites in the veins where blood flow is reduced.

For a clearer picture, doctors use phlebography in diagnostics. The veins in the uterus are filled with a substance that provides contrast during fluoroscopy.
The difficulty of diagnosis, along with mild symptoms, is the lack of a specific site of localization, the pelvic return.
If diagnosed by a doctor, varicose veins can be confused with a common inflammatory process, the likelihood of such a defect being particularly high in the early stages.
Important!If your gynecologist has diagnosed inflammation and prescribed therapy, but this does not help you cope with the symptoms, we need to understand that this effect is not normal and it is imperative to visit a specialist.
You can make a correct diagnosis with confidence with the following methods:
- Doppler ultrasound;
- Phlebography - diagnoses varicose veins quite accurately;
- Ultrasound of the venous system - vaginal examination or transdomdominal scanning is used in various situations;
- Laparoscopy - this method allows you to identify varicose formations in the ovaries as well;
- Selective ovarian examination - this diagnostic method is most likely used to detect varicose veins in the small pelvis. To do this, contrast fluid is injected into the veins of the thigh and subclavian region.
If the diagnosis is not accurate, the patient may be referred for further examination. A blood test is prescribed.
Classification of the extent of the disease
Depending on the stage and severity of pelvic varicose veins, it can be divided into three categories. The location of venous dilatation is also an important parameter in this regard.
- Pelvic varicose veins inflate the veins to 5 mm in the first stage due to the appearance of a small number of deformed areas;
- In the second stage, the veins are 6-10 mm in diameter and loose ectasia of the plexus occurs in the ovary;
- The last degree is the most dangerous, the patient's venous swelling exceeds a volume of 10 mm. The third degree of damage is characterized by the parametric localization of the main type.
After successful diagnosis and diagnosis of the disease, appropriate treatment of varicose veins is prescribed.
Conservative treatment methods

It is best to consult the appropriate professionals after making an accurate diagnosis. Diseases associated with varicose veins are treated by a phlebologist. You can only receive a referral after the gynecologist has made the diagnosis and the pelvic dilatation of the men has been confirmed by a urologist.
The main tasks that put the doctor on the path to recovery are:
- Restoring damaged venous walls and restoring their normal tone;
- Prevention of subsequent stagnation in the pelvic veins;
- Improving the condition of venous tissue.
Complex therapy is used to solve the set tasks, which includes a special diet, rehabilitation exercises, medications for treating varicose veins, and the use of special styling underwear.
Therapeutic phase of treatment
The main goal of pelvic varicose vein therapy is to restore blood flow and normalize the tone of elastic tissues. The stages of removing the unpleasant symptoms of the disease and increasing the blood circulation in the veins are no less important.
Antiviral drugs should only be prescribed by a phlebologist. Two groups of drugs are prescribed for the disease. The first (venotamic drugs) - improves the tone of vein tissues, the second (angia aggregants) - prevents the formation of new blood clots.
In case of exacerbation of pelvic varicose veins, taking medications in the courses is an important therapy. Venotonic drugs, which improve vascular tone, play a major role in treatment. To prevent recurrence of the disease, these drugs are prescribed for prophylaxis.
Medications for the treatment of pelvic varicose veins should only be prescribed by a doctor, self-medication is unacceptable!

Generally, anti-varicose drugs contribute to:
- Stop blood flow;
- Normalize venous tone;
- Help blood supply to tissues;
- Reduction of the discomfort associated with the symptoms of the disease.
It should be remembered that the use of medicines should be combined with special exercises and a prescribed diet.
Traditional Medicine
Folk methods are often used to treat pelvic varicose veins, the main cures of which include herbal infusions that restore normal vein tone. The most popular decoctions are the roots of horse chestnut, chaga and dandelion.
Hirudotherapy is well-established in humans: leeches should be used in the sacrum and coccyx region.
Important to know!It is impossible to allow a varicose vein excavated in a pelvis to drift or to rely solely on the tools of traditional medicine. This rather dangerous disease should be treated in a comprehensive way, with mandatory intake of medications, and the use of infusions and decoctions should only be an adjunct.
Preventive Tournament
There are several exercise techniques to restore tissue tone.
- Raising and lowering the toes, the exercise is performed in a standing position, the number of repetitions is at least 30, the toes and heels are parallel;
- The same will be enough just spreading the socks and adjusting the heel 30 times;
- Repeat the toe pull, maximizing the heel and aligning the toes;
- Varicose vein breathing exercises can be treated by slowing it down, imagining how all the abdominal muscles are affected;
- In a prone position, lift the pool with your hands and perform a "cycling" move. For those who find this practice difficult, they can replace them with a "birch tree" or take turns.

Physiotherapy is good if the veins in the small pelvis are dilated and comfortable to perform anywhere. The main condition for success will be the regularity of performing special exercises, but by no means should the hours be overloaded.
It is just as important to follow a healthy lifestyle if you have been diagnosed with venous dilatation. Take regular breaks from physical work, and if this involves a long stay in a static position, you should take breaks, warm up, and walk periodically.
A good solution would be to use a contrast shower, varicose veins will cause discomfort in the perineal area, so there will be no need to direct the flow of water to this area.
Proper nutrition
It is important to create a diet that does not have bowel movements, especially constipation. With these, venous expansion may be exacerbated by an increase in internal pressure during bowel movements. It is better to avoid eating too spicy and fatty foods as these affect blood clots.
Nutritional correction for pelvic varicose veins includes the exclusion of saturated fatty foods and alcoholic beverages. In the diet, preference should be given to high-fiber foods (vegetables and fruits, cereals), healthy fats (vegetable oils).
Once you have learned from your doctor how to treat pelvic varicose veins and what food restrictions to apply, you need to take care of your general body condition by doing well to get rid of bad habits (smoking and alcohol) during rehabilitation.
Possible complications
Varicose veins in the pelvic organs can cause serious complications for the female body, especially in the later stages of the disease. Sometimes the inflammation spreads to adjacent organs, uterine bleeding seems scarier.
For better protection, you need to understand the risk of pelvic varicose veins. Frequent bleeding in the uterus can contribute to thrombosis and develop into an extensive inflammatory process.
Forecast
In women, pelvic varicose veins can contribute to severe consequences, but most often occur at later stages due to late detection of the disease. Therefore, attention should be paid to pelvic varicose pain, as these are the most obvious symptoms, indicating that a doctor should be consulted.























